If you've had Hashimoto's for any period of time you've probably at least heard some mention of Hashimoto's and gluten being incompatible. I'm constantly seeing heated debates on Facebook groups and forums about whether or not to avoid gluten if you have Hashimoto's. There's been a lot of noise about the topic lately because unfortunately, the two are becoming increasingly linked.
Gluten is a group of storage proteins that includes glutenin and gliadin and is present in foods like wheat, barley, and rye. Hashimoto's thyroiditis is an autoimmune disease affecting the thyroid gland. When the thyroid is attacked, hormone levels drop, leading to hypothyroidism (underactive thyroid).
You may be wondering if it's necessary to give up gluten. This post will explore the link between Hashimoto's and gluten consumption and get into some of the research.

What is Gluten?
Gluten is found in wheat, rye, barley, and triticale. It is made up of two proteins called glutenin and gliadin. Gluten acts as a glue that keeps foods together, allowing them to keep their structure.
It is often added to processed foods to increase texture and moisture retention due to its unique physical qualities. Gluten proteins produce a sticky network with a glue-like consistency when flour is mixed with water.
Gluten is plentiful in the American diet as it's found in practically everything from bread to pasta to crackers, hotdogs, lunchmeats, soups, sauces, etc.
Gluten is a controversial topic these days. Some consider it safe for everyone except celiac disease patients. However, others, including some health professionals, believe that gluten is hazardous to the majority of people.
**Just a quick heads up- this post contains affiliate links which means if you click on them and buy something, I will earn a small commission (at no additional cost to you) to help continue maintaining this site.
Note to readers: This site does not provide medical advice. It is intended for informational purposes only. It is not a substitute for professional medical advice, diagnosis or treatment. Consult your doctor before making any medical decisions.
What is Hashimoto's Thyroiditis?
Hashimoto's disease is an autoimmune disorder affecting the thyroid. Roughly 90 percent of hypothyroidism cases are caused by Hashimoto's. [1]. Hyperthyroidism, or an overactive thyroid, can occur as well though it's less common.
The thyroid gland is a tiny butterfly-shaped gland located at the front of the neck. The immune system creates antibodies that attack the thyroid gland, causing excessive numbers of white blood cells, which are part of the immune system, to start building up in the thyroid. This buildup leads to thyroid damage and a reduced ability to make enough thyroid hormones.
Thyroid hormones regulate how your body uses energy; therefore, they impact the function of pretty much every organ in your body, including how your heart beats.

Link Between Hashimoto's and Gluten
Gluten-free diets have become increasingly popular among people with Hashimoto's and other autoimmune diseases. This is largely a result of the growing concern that gluten contributes to Hashimoto's development and progression.
Above, we talked about antibodies that attack the thyroid and cause damage in people with Hashimoto's. It turns out that the protein structure of gluten is similar to the structure of the thyroid, so it is believed that when someone with Hashimoto's disease eats gluten, those antibodies react.
Since high antibody levels are linked with increased Hashimoto's symptoms, reducing antibody levels may help reduce some of these symptoms. [2]
Research has been able to show a strong correlation between gluten intolerance and Hashimoto's disease. Celiac disease is a condition in which gluten causes an autoimmune response in the stomach, skin, or neurological tissue in certain people.
Gluten intolerance (or gluten sensitivity) is more common than celiac disease, but both are more prevalent in Hashimoto's hypothyroidism patients than in the general population. [3]
One small trial of 34 women with Hashimoto's disease showed that following a gluten-free diet for 6 months did reduce antibody levels, but further research is needed to validate these findings [4].
How Does Gluten Affect the Body and Thyroid?
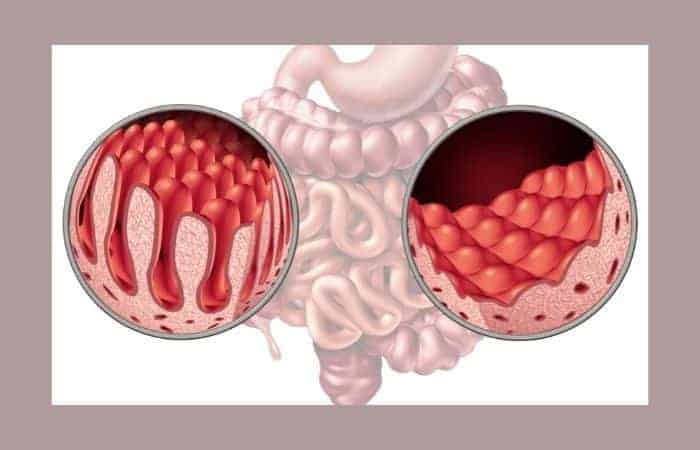
In someone with Celiac disease, gluten causes an immunological response. When those with Celiac disease eat gluten-containing foods, their digestive tracts and other parts of the body become inflamed and damaged.
Even without Celiac disease, some people react negatively to gluten. Their bodies sense it as a toxin and their immune system overreacts in response to it. If a gluten-intolerant person continues to eat gluten, it creates an inflammatory environment.
Your small intestine plays a huge role in your health. It is responsible for absorbing the majority of the nutrients from your diet and ensuring that your body receives the energy and nutrition it requires. It also houses a significant portion of your immune system.
When people with celiac disease eat gluten-containing foods, their small intestine can become inflamed and damaged. As a result, it can eventually lead to malabsorption, a condition in which your body is unable to obtain the nutrients it requires from your small intestine.
Gluten Sensitivity vs Celiac Disease vs Wheat Allergy
Gluten sensitivity, gluten intolerance, wheat allergy, and Celiac disease are terms that are thrown around a lot. However, they don't all mean the same thing, so it's worth explaining.
After ingesting gluten, two people may experience the same symptoms - bloating, stomach discomfort, and diarrhea, but they may have two separate gastrointestinal (GI) diseases: celiac disease and gluten intolerance, or non-celiac gluten sensitivity (NCGS). Then there's the third person who has a wheat allergy...let's get into it below.
There are actually 3 potential ways people can react to gluten:
1. Wheat Allergy (allergic reaction)
This is an IgE immune response that causes immediate and obvious allergic reactions like anaphylaxis, trouble breathing, rashes, etc. It can occur in response to glutenin, gliadin, or other components of wheat. [5]
2. Celiac Disease
Celiac disease is an example of a delayed hypersensitive response to gliadin in wheat. It can be IgA, IgG, or T-cell mediated, take several days to develop, and involves tissue transglutaminase. This type of reaction causes damage to the intestines in people that are genetically susceptible. Tissue transglutaminase is an enzyme found in many cells in the body. It is released into the bloodstream when intestinal damage occurs. That's why transglutaminase antibodies are one thing used to diagnose Celiac disease via a blood test.
Celiac disease affects about one in every 100 people worldwide. [6] In fact, the incidence of Celiac disease is increasing at a rate of about 7.5% per year! [7] A gluten-free diet is the only treatment option for this condition.
When a person with celiac disease consumes even trace amounts of gluten, their immune system attacks the lining of the small intestines often leading to issues like bloating, diarrhea, nutritional deficiencies, etc. Some people with Celiac disease have zero symptoms, yet the damage is still occurring.
3. Gluten Intolerance, Gluten Sensitivity, Non-Celiac Gluten Sensitivity (NCGS)
These three terms are often used interchangeably and basically mean the same thing. They also result from a delayed hypersensitive reaction to gluten as mentioned above, but they can happen in someone without celiac disease. This can be caused by loss of immune tolerance to gluten or leaky gut. [8] In the case of a leaky gut, food particles get into the bloodstream causing an IgG or IgA systemic response. [9]
Gluten intolerance is a sensitivity vs. Celiac disease which is an autoimmune disorder. A person with gluten intolerance, also known as non-celiac gluten sensitivity, can exhibit symptoms that are similar to celiac disease. While both disorders cause the body to react adversely to gluten, the two types of responses are not the same in terms of duration or consequences. [10]
When someone with Celiac disease eats gluten, their immune system attacks their own body tissues. If someone is gluten intolerant, however, eating gluten will result in short-term bloating and stomach pain. Gluten intolerance, unlike celiac disease, does not usually cause long-term damage to the body.
How to Test For Gluten Sensitivity
Gluten sensitivity is difficult to test for. People who have digestive symptoms that could indicate celiac disease should consult a gastroenterologist to see if they are at risk for celiac disease or gluten sensitivity. A negative celiac disease test does not eliminate the possibility of gluten intolerance.
Celiac antibody tests are simple blood tests used to screen for celiac disease. However, you must be eating gluten in your diet for a period of time before the test for it to be accurate. [11] The blood test is able to detect specific antibodies in the blood that the immune system produces in response to gluten.
To gauge your sensitivity to gluten, the most common strategy is to take it out of your diet for at least a few weeks to see if your digestive symptoms improve. Gluten sensitivity may be the cause of your symptoms if they improve on a gluten-free diet but return when you eat gluten-containing foods.
Can a Gluten-Free Diet Improve Hashimoto's Symptoms?
Anecdotally, I've heard many people say that adhering to a gluten-free diet vastly improved their autoimmune symptoms. Of course, it's important to look into the science and validity of this as well. Research is still developing in this area but we are learning more and more about how gluten affects human health. We are increasingly seeing indications that avoiding gluten can positively affect thyroid health if you have Hashimoto's.
According to one study, 29 percent of patients with non-celiac wheat sensitivity (NCWS) and 29 percent of patients with celiac disease developed an autoimmune condition, the most common of which was Hashimoto's thyroiditis [3].
A recent pilot study sought to determine if a gluten-free diet had any effect on autoimmunity in Hashimoto's patients. After six months, the gluten-free diet group had lower thyroid antibody titers and somewhat higher 25-hydroxyvitamin D levels. [4] This implies that a gluten-free diet may indeed be beneficial for those with Hashimoto's.
Molecular Mimicry

Although further research is needed, molecular mimicry may be responsible for the relationship between Hashimoto's and gluten. [12] When molecular mimicry occurs, the body generates antibodies against a target that has a similar peptide structure but is molecularly different from the molecule the body is primed to target.
Gluten and thyroid tissue have similar peptide structures, or physical shapes, which could be triggering a cross-activation immunological response. Picture a key that is so similar to another key that it can open a door it wasn't designed to open.
Do I Have to Stay Completely Gluten-Free?
The truth is that people's reactions to gluten are exceedingly diverse. As a result, establishing a safe threshold level is difficult. People with celiac disease and non-celiac gluten sensitivity (NCGS) should avoid gluten intake.
With celiac disease, the only treatment is a lifelong gluten-free diet. Gluten-free diets help the villi in the small intestine to repair, resulting in better nutritional absorption. Symptoms will fade over time.
Gluten avoidance is critical for celiac disease management. Even if you don't have symptoms, consuming gluten daily might cause damage to the small intestine. If the diet is strictly followed, the chance of long-term problems, such as gastrointestinal cancer, is considerably reduced. [13]
If you have Hashimoto's and gluten intolerance, eliminating gluten from your diet is often advised. Even cheats and small bites can activate an immunological response that damages thyroid tissue.
Conclusion
There is growing evidence that it's likely a good idea to avoid gluten if you have Hashimoto's. Consult your doctor about the possibility of celiac disease if you have an autoimmune disorder. If you suspect you might have a gluten intolerance, it may help to exclude it from your diet for a while to see if it makes a difference in how you feel. If you want to get more aggressive with tackling an autoimmune-friendly diet (which includes eliminating gluten), check out my Beginners Guide to the Autoimmune Protocol.
If you enjoyed this post, you may also like:
Don't Get Glutened- Ways to Protect Yourself
- References:
- Amino N. Autoimmunity and hypothyroidism. Baillieres Clin Endocrinol Metab. 1988 Aug;2(3):591-617. doi: 10.1016/s0950-351x(88)80055-7. PMID: 3066320.
- Ana Barić, Luka Brčić, Sanda Gračan, Veselin Škrabić, Marko Brekalo, Marta Šimunac, Vesela Torlak Lovrić, Iva Anić, Maja Barbalić, Tatijana Zemunik, Ante Punda & Vesna Boraska Perica (2019) Thyroglobulin Antibodies are Associated with Symptom Burden in Patients with Hashimoto's Thyroiditis: A Cross-Sectional Study, Immunological Investigations, 48:2, 198-209, DOI: 10.1080/08820139.2018.1529040
- Carroccio, A., D'Alcamo, A., Cavataio, F., Soresi, M., Seidita, A., Sciumè, C., ... & Mansueto, P. (2015). High proportions of people with nonceliac wheat sensitivity have autoimmune disease or antinuclear antibodies. Gastroenterology, 149(3), 596-603.
- Krysiak, R., Szkróbka, W., & Okopień, B. (2019). The effect of gluten-free diet on thyroid autoimmunity in drug-naive women with Hashimoto's thyroiditis: A pilot study. Experimental and Clinical Endocrinology & Diabetes, 127(07), 417-422.
- Vojdani A, O'Bryan T, Kellermann GH. The Immunology of Immediate and Delayed Hypersensitivity Reaction to Gluten. European Journal of Inflammation. January 2008:1-10. doi:10.1177/1721727X0800600101
- Mahadov S, Green PH. Celiac disease: a challenge for all physicians. Gastroenterol Hepatol (N Y). 2011;7(8):554-556.
- King, James A. MSc1; Jeong, Jocelyn MD1,2; Underwood, Fox E. MSc1,3; Quan, Joshua3; Panaccione, Nicola3; Windsor, Joseph W. PhD1,3; Coward, Stephanie PhD1,3; deBruyn, Jennifer MD2; Ronksley, Paul E. PhD1; Shaheen, Abdel-Aziz MBChB1,3; Quan, Hude PhD1; Godley, Jenny PhD4; Veldhuyzen van Zanten, Sander MD5; Lebwohl, Benjamin MD6,7; Ng, Siew C. PhD8; Ludvigsson, Jonas F. MD9,10; Kaplan, Gilaad G. MD, MPH1,3 Incidence of Celiac Disease Is Increasing Over Time: A Systematic Review and Meta-analysis, The American Journal of Gastroenterology: April 2020 - Volume 115 - Issue 4 - p 507-525
doi: 10.14309/ajg.0000000000000523 - Molberg Ø, Sollid LM. A gut feeling for joint inflammation - using coeliac disease to understand rheumatoid arthritis. Trends Immunol. 2006 Apr;27(4):188-94. doi: 10.1016/j.it.2006.02.006. Epub 2006 Mar 10. Erratum in: Trends Immunol. 2006 Jun;27(6):254. PMID: 16530013.
- Vojdani A, O'Bryan T, Kellermann GH. The Immunology of Immediate and Delayed Hypersensitivity Reaction to Gluten. European Journal of Inflammation. January 2008:1-10. doi:10.1177/1721727X0800600101
- Pietzak, M. and Kerner, J.A., Jr. (2012), Celiac Disease, Wheat Allergy, and Gluten Sensitivity. Journal of Parenteral and Enteral Nutrition, 36: 68S-75S. https://doi.org/10.1177/0148607111426276
- N. Ontiveros, M. Y. Hardy, F. Cabrera-Chavez, "Assessing of Celiac Disease and Nonceliac Gluten Sensitivity", Gastroenterology Research and Practice, vol. 2015, Article ID 723954, 13 pages, 2015. https://doi.org/10.1155/2015/723954
- Ihnatowicz P, Wątor P, Drywień ME. The importance of gluten exclusion in the management of Hashimoto's thyroiditis. Ann Agric Environ Med. 2021;28(4):558-568. doi:10.26444/aaem/136523. Marafini I, Monteleone G, Stolfi C. Association Between Celiac Disease and Cancer. Int J Mol Sci. 2020 Jun 10;21(11):4155. doi: 10.3390/ijms21114155. PMID: 32532079; PMCID: PMC7312081.


Leave a Reply